Cervical Screening
What is the Cervical Screening Test?
The Cervical Screening Test (CST) aims to prevent cancer of the cervix (also called cervical cancer). Cervical cancer is preventable with regular cervical screening because pre-cancerous changes can be found and easily treated, so cancer does not develop.
Most people who do develop cervical cancer have either never had cervical screening or have had screening less often than recommended. Cervical screening saves lives!
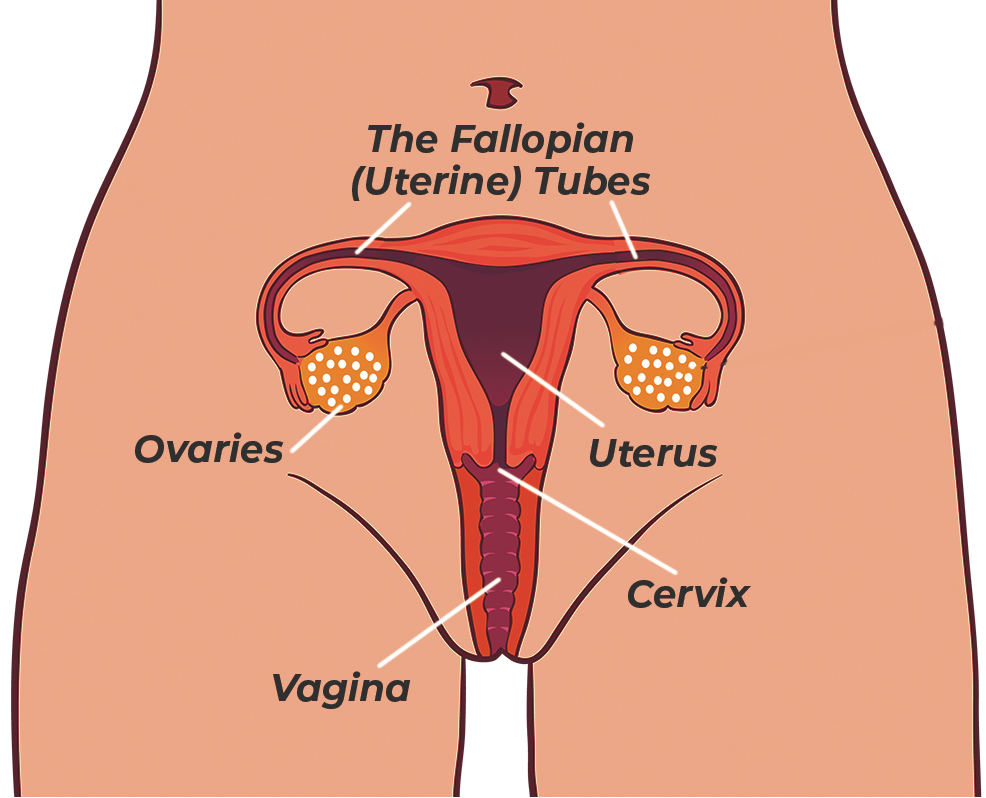
What is the cervix and where is it?
The cervix is the lower part of the uterus (womb) and is at the top of the vagina.
What does the Cervical Screening Test do?
The Cervical Screening Test looks for the Human papillomavirus (HPV). We now know that HPV causes over 99% of cervical cancer. The Cervical Screening Test is more accurate and has replaced the Pap test.
What is HPV?
HPV is a large group of viruses that commonly affect humans. Most HPV types are harmless, however 14 HPV types can cause cell changes that, if left untreated, can potentially cause cancer. HPV types 16 and 18, cause the majority of cervical cancer.
How do you get HPV?
You get HPV through sexual activity. HPV is common, and almost everyone who has ever had sex is exposed to it. You do not need to have had sexual intercourse to become infected with HPV; it can occur just through close genital skin-to-skin contact. Most people clear HPV themselves without needing any treatment.
Who should have a Cervical Screening Test?
All women and people with a cervix aged between 25 and 74 years and who have ever been sexually active should have a regular Cervical Screening Test.
Including:
- If you have only ever had one sexual partner in your life
- If you are no longer sexually active
- If you are post-menopause
- If you identify as lesbian, transgender, intersex, non-binary, or queer
- If you are pregnant
- If you have had a baby
- If you have had the HPV vaccine (the vaccine does not protect against all HPV types)
What happens during my appointment?
The nurse or doctor will talk with you first, ask you some questions about your health and your past cervical screening results, and will explain your choices. There are now two ways of having a cervical screening test: clinician-collected and a self-collected.
What if I am worried, frightened, or embarrassed about having the test?
The Cervical Screening Test is a simple and quick procedure. If you have never had a Pap smear or Cervical Screening Test, ask your doctor or nurse to explain what will happen and to show you the speculum.
If you are anxious or concerned about having the procedure, consider calling us or making an appointment to discuss your concerns first.
Remember that the nurses and doctors at Sexual Health & Family Planning ACT are specially trained and highly experienced in cervical screening. They do these tests all the time, and work to make the experience a safe and positive one for you. You can also choose to have a self-collected Cervical Screening Test.
The clinician-collected Cervical Screening Test
You can choose to have a clinician-collected Cervical Screening Test, and if you have symptoms or have had a recent abnormal test, then it is recommended that you do this. A clinician-collected Cervical Screening Test is when the nurse or doctor collects the sample.
To do this they will invite you to take off your clothes from the waist down, including underwear, and ask you to lie down on an examination bed. You can leave your top on and should be offered a privacy sheet to cover up if you want it.
The nurse or doctor will then gently insert a small instrument called a speculum into the vagina so that they can see the cervix. They will use a soft brush to collect cells from the cervix and place the sample into a container. The test itself should only take about 5 to 10 minutes.
The sample is then sent to the pathology lab to check for HPV and to look at the cells if needed.
The self-collected Cervical Screening Test
You may choose to collect your own sample. This is called a self-collected Cervical Screening Test. The self-collected cervical screening test is done after talking to a nurse or doctor. Not everyone is eligible to have a self-collected test (for example, if you have symptoms), so you will need to check with your doctor or nurse.
• How do I do a self-collected cervical screening test?
The test is simple to do. You will be given a red topped tube with a long cotton tip swab. You do the test in a bathroom or other private space. Wash your hands with soap and water and dry them well. Remove your underwear, twist the red cap, and remove the swab from the tube. Locate the red mark halfway down the swab, part the skin folds at the opening of your vagina and insert the swab into your vagina up to the red mark. Gently rotate the swab for 20-30 seconds. Remove the swab from your vagina, put it back into the tube, and return it to your nurse or doctor.
• Is the self-collected test accurate?
Yes, the self-collected test is just as accurate as the test collected by a nurse or doctor using a speculum. The main difference is that when a nurse or doctor collects the sample, they can collect cells. They are also able to examine your vulva, vagina, and cervix. Some conditions, such as polyps, inflammation, or skin conditions, can only be diagnosed when seen on examination.
• What happens if HPV is detected on my self-collected test?
If HPV is detected, it depends on what type it is as to what happens next.
- If type 16 or 18 are detected, you will be referred to a gynecologist for further investigation.
- If one of the other HPV types is detected, you will need to return to your nurse or doctor to have a speculum examination so they can collect a sample of cells from the cervix. Collecting cells is essential as it will guide what happens next and if you need to see a gynaecologist or just return for a repeat test in 12 months.
If you are under 30, there is around a 17% chance that you will need to return for a clinician-collected sample (this is because HPV is more common in younger people). If you are over 30, there is around a 5% chance that you will need to return.
• What about home self collected tests
Several ‘self-testing’ home-based kits are being advertised in Australia that are not part of the National Cervical Screening Program. These are not approved and should not be used.
What do my test results mean?
Cervical Screening Test results include low-risk, intermediate-risk, and higher-risk.
- Low Risk: This means that no HPV was detected, you are at low risk of developing any abnormality, and you do not need another test for five years. If you have any symptoms (such as bleeding after sex or between periods) before your next test is due, you should always see a doctor.
- Intermediate Risk: If your test result shows HPV types (not 16 or 18) and the cells are normal or only mildly abnormal, you will need to return for another HPV test in 12 months. If the virus is still present on your second test, you will be asked to repeat the test in another year. It is usual to take 1-2 years to clear the HPV. However, if you have had a self-collected test that shows HPV (types not 16 or 18) you will need to return to see your nurse or doctor so they can collect a sample of cells from the cervix. Self-collection is excellent for picking up the presence of HPV but cannot pick up cells that may have changed as a result of HPV.
- Higher Risk: If your test result shows HPV type 16 or 18 (or other HPV types and the cells show significant changes), this means that you are at higher risk of developing an abnormality. You will need to be referred to a gynaecologist for further investigation.
What if I am under 25?
If you are under 25 and have already had a normal Pap smear in the past, then you only need to have a Cervical Screening Test when you turn 25. If you are under 25 and have not yet had any cervical screening, you will be invited to participate in the program when you turn 25.
Is it safe for me to wait until 25 for my first test?
Yes, it is safe because:
- Cervical cancer is very rare in people under 25
- Most young people will clear the virus themselves
- Starting at age 25 means that we avoid unnecessary tests and treatment in young people
- Most young people are protected by the HPV vaccine, which reduces the risk of any abnormalities developing
If you did not receive the HPV vaccine and had any sexual activity before 14 years of age, you can ask your doctor or nurse about having a Cervical Screening Test at an earlier age.
What if I am 75 or older?
If you had your last CST between the age of 70-74 and the result was normal (Low Risk), you can stop cervical screening. However, you can continue to screen every five years from 75 if you wish to.
How will I know when my Cervical Screening Test is due?
The National Cancer Screening Register keeps all cervical screening results. They will send you a reminder in the mail when your next test is due and a second reminder if you do not attend for screening on time. The clinic where you have your regular Cervical Screening Tests may also send you a reminder.
What if I have symptoms?
Please remember that the routine Cervical Screening Tests are for people with no symptoms. If you have any symptoms, they need to be investigated, so you will need to see a doctor.
Symptoms include:
- Unusual vaginal bleeding (after sex or between your periods)
- Any vaginal bleeding after menopause
- Unusual and unexplained vaginal discharge that doesn’t go away
- Pelvic pain
- Pain with sex